What keeps you awake at night? Well, for veterans, there are any number of factors that could be contributing to insomnia including traumas associated with deployment, years of irregular work hours and the difficulties surrounding the transition into civilian life. Just to name a few. But now, a growing number of post-9/11 veterans and military families are learning how to trade in tossing and turning for deep sleep with the help of Cognitive-Behavioral Therapy for Insomnia (CBT-I.) A sleep specific therapy, CBT-I has been shown to improve sleep in 75 to 80% of individuals with insomnia.
CBT-I works by identifying and changing thoughts and behaviors that prevent restful, quality sleep and is usually effective within 6-8 weekly sessions. Sleep-medicine specialist Philip Gehrman, PhD, an associate professor of psychiatry at the University of Pennsylvania, says that often when people develop chronic insomnia their bodies get stuck in a cycle. He adds, “CBT-I is really the only treatment designed to break that cycle and establish a healthy pattern of sleep again.” As we approach Sleep Awareness Week – March 14th to 20th, 2021, let’s take a look at a few key components to the treatment:
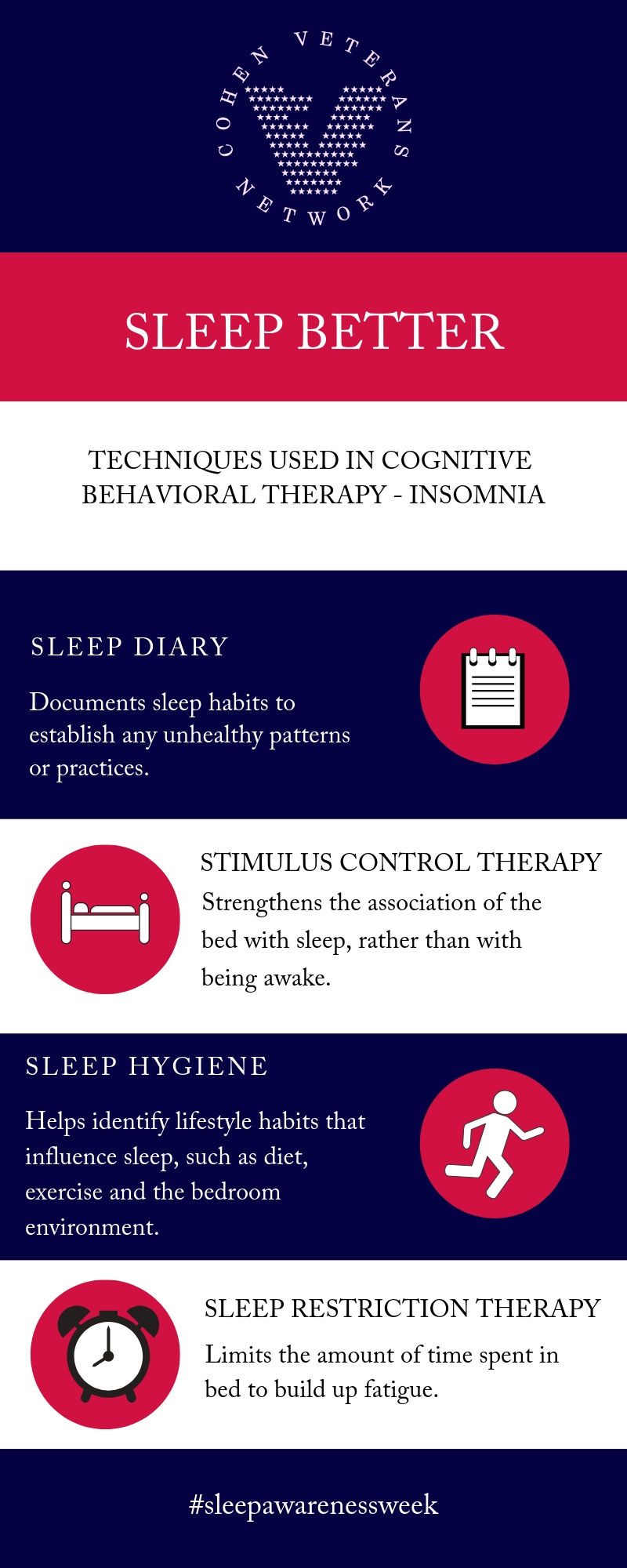
A Sleep Diary: As a first step in CBT-I, clients are asked to keep a sleep diary to help assess their sleep patterns and behavior. “Each morning when they get up for the day they’re supposed to answer a series of questions about how they slept the night before. Such as, what time they went to bed, how long it took to fall asleep, how long they were awake in the middle of the night etc.,” notes Gehrman. The sleep diary will then be used to help determine the best treatment for the client.
Stimulus Control: “Stimulus Control is designed for one specific type of disruption. It’s what we call a ‘conditioned’ or ‘learned arousal pattern.’ When people are good sleepers, each night they get into bed and they fall asleep and that happens night after night. Their body just learns an association between being in bed and sleep. For people who are good sleepers when they get into bed it often triggers this automatic reaction or response of starting to feel more sleepy. People with insomnia have generally spent months and years not sleeping well in bed. Their body has learned to connect the bed as a place for wakefulness rather than sleepiness. For a lot of people with insomnia they are tired at night,” Gehrman explains. “But then they get into bed and start feeling more wide awake. It’s a very frustrating aspect of insomnia, and it’s one of the biggest factors that tends to keep it going over time. It’s all based on the idea that we’re trying to teach people how to retrain their bodies to connect the bed with sleep rather than with wakefulness.”
Sleep Hygiene: Sleep hygiene focuses on the basic lifestyle habits that influence sleep, such as diet, exercise, caffeine intake etc. Additionally, it looks at clients’ sleep environments. Gehrman says, “It includes looking at their bed and bedroom. Asking, is it conducive to sleep?”
Sleep Restriction Therapy: This technique reduces the amount of time a client spends in bed. Gehrman says, “The most challenging component of the treatment is the sleep restriction because we’re basically purposely using mild sleep deprivation to our advantage. We’re restricting people’s time in bed to build up what we call ‘sleep drive.’ The idea with this is that the longer you’re awake a drive for sleep builds up. Just like the longer you go without eating, hunger builds up. Sleep works the same way. So, we’re building up sleep drive a little bit night after night after night. People reach this tipping point in which the time they’re in bed the quality of that sleep starts to improve. The way sleep restriction works is we worry about the quality of sleep before we worry about the quantity.”
Learn more about CBT-I, here.
By Kate Sullivan,
Manager, CVN Newsroom
